Sleep Better: Break the Cycle of Bad Sleep
There is a sleep crisis.
A qualitative analysis of nurses revealed that 92% of participants reported at least one sleep problem, of which 68% were insomnia-related problems (1). So this is probably you. It’s definitely someone you work with or get report from every day. Additionally, an increased rate of burnout positively correlates to an increase in sleep issues (2) and 65% of nurses report being burned out (3). A common symptom of burnout is chronic exhaustion.
When I worked as a staff nurse, one of my clues that life needed to change was that I was ALWAYS chasing MORE energy. I only had enough to just survive and barely function, but I was not living. Frequently, I woke up more tired than when I went to sleep. But I didn’t understand why.
Now I do.
There’s the biology underlying your sleep issues that are influenced by the chronic stress you experience at work and home
A deeper understanding of the biology leads to aligning with your natural sleep rhythms by creating targeted and effective tools to get better & restorative sleep
These tools are actionable steps that when integrated into your daily life lead to better regulated hormones. And your life is ruled by your hormones
And this is adaptable to your swing or night shift by creating an effective Wind Down sleep routine
Picture of Doris Taylor, RN (author) as an exhausted staff nurse with dark circles under eyes, taken at work in Seattle, WA.
Restorative Sleep
We crave it but what is it?
Only during sleep is the body able to repair itself. Not just the body but also the mind, thereby promoting physical and mental well-being. This occurs just in stages 3 and 4 of sleep, which are the deep and the rapid eye movement (REM) phases.
Stage 3: Deep Sleep
The body repairs and regrows tissue, builds bone and muscle, and strengthens the immune system. This stage lasts about 20-40 minutes, your heartbeat and breathing are at their slowest, no eye movement and your body is fully relaxed.
Stage 4: REM sleep
The stage where you typically dream, is essential for learning, memory, and cognition. This stage lasts anywhere from 10-60 minutes. Your brain activity is similar to when you are awake, you have rapid eye movement (brain processing) and faster breathing and heart rate. The body cycles through all four stages approximately 4-6 times per night, averaging 90 minutes for each cycle.
Non-restorative sleep is when you wake up feeling unrefreshed despite having slept the recommended number of hours. Or more hours, or even less but you still wake up exhausted and sluggish.
4 sleep cycle stages
Stage 1: Falling Asleep
This is the lightest stage of sleep and lasts 1-7 minutes. Comprising only 5% of total sleep time.
Stage 2: Light Sleep
This stage represents progressively deeper sleep as the heart rate and body temperature drop.
Your brain waves slow down and have noticeable pauses between short bursts of electrical activity. Experts believe these bursts is the brain organizing memories and information from the time you were awake.
In the first cycle, this stage lasts around 25 minutes and lengthens with each successive cycle, eventually comprising 45% of total sleep.
If you grind your teeth (bruxism), this is the stage it will happen.
Insomnia
One-third of adults experience acute insomnia and one in 10 suffer from chronic insomnia (6).
Is defined as difficulty falling asleep (taking more than 30 minutes), trouble staying asleep (waking up in the middle of the night), waking too early despite adequate opportunity for sleep and non-restorative sleep. Symptoms occur at least 3 nights per week for at least 3 months (becoming chronic insomnia). This might occur because of hormonal changes (adolescence, perimenopause and menopause), children, stress, life changes, trauma, and/or your work schedule.
There are two types:
Insomniac on phone sitting up in bed late at night
Primary: not caused by another condition
Idiopathic insomnia is truly without any identifiable contributory factor (4)
Stress-related insomnia can be characterized by mild stress, such as rumination or other thoughts throughout the night (4)
Sleep state misperception (SSM), also known as paradoxical insomnia. A person feels that they are experiencing insomnia, although they are getting enough sleep and don’t experience daytime signs of sleep deprivation (4)
Secondary: caused by another medical or psychological condition, medication or substance. It is the most common form of insomnia, accounting for approximately three-quarters of cases seen in both patient and general populations (5)
Navigating the Shadowlands
Not sleeping has a profound impact on your well-being. There is an impact on memory, mood, neuro-protective functions (that occur during restorative sleep). It will impact your relationships and can have an economic impact (due to real or perceived work productivity reduction). You may experience anxiety, rumination or dread in the middle of the night. It becomes your own personal nightmare. During the day you have fatigue, feel crappy, eat poorly, don’t exercise, drink to relax and stay up late bingeing a show or scrolling social media. Rinse & repeat daily.
Cardiometabolic & Inflammatory Impact
Cardiometabolic is the health of both the cardiovascular system and the metabolic system. It encompasses the risk factors and conditions that can lead to heart disease, stroke, type 2 diabetes, and other related health issues.
Metabolic Disruption
Impaired glucose metabolism and reduced insulin sensitivity
Increased risk of insulin resistance and potential progression to Type 2 Diabetes Mellitus
Weight Dysregulation
Hormonal imbalance leading to increased appetite
Increased cravings for caloric-dense foods and potential for decreased physical activity
Contributes to weight gain & increased risk of obesity
Cardiovascular Health Risks
Increased risk of hypertension, coronary artery disease, heart attack and stroke
Disruption of night time blood pressure dip and increased inflammation
Cognitive Impairment
Impaired memory consolidation and recall
Reduced problem solving and decision-making abilities
Potential link to increased risk of long-term cognitive decline (80% of Alzheimers occurs in women)
Person in white coat and stethoscope asleep at desk with coffee in hand
Psychological Factors
Stress & Anxiety
Stressful life events or chronic worry and rumination keep the mind active making it hard to fall asleep and/or stay asleep
Depression
Insomnia and depression frequently co-exist, it’s not always clear which came first
Negative Sleep-Related Beliefs
People with insomnia can develop negative beliefs and expectations about sleep, such as fearing that they will never be able to sleep or that they will be exhausted all day.
These beliefs can create a self-fulfilling prophecy, leading to increased anxiety and difficulty sleeping.
Exhausted & anxious unicorn
Personality Traits
Neuroticism, characterized by a tendency to experience negative emotions and perceive the world as threatening, has been linked to insomnia.
Dysregulated Nervous System
A hyper- and hypo- aroused state will disrupt your sleep. For more detailed information, read this Connecting The Dots article
Parenting & Family Stress
Young kids, older kids, adult children
Taking care of older parents
Toxic family dynamics
Perimenopause & Menopause (10)
Hormonal fluctuations during menopause can contribute to mood swings, anxiety and depression. These conditions are often associated with difficulty falling asleep, staying asleep and early morning waking
Women with pre-existing anxiety disorders are twice likely to develop severe insomnia during the menopausal transition
There is a bi-directional relationship between sleep & mood
Perfectionism, hyper-vigilance and “3 AM Thought Spirals”
Physiological Factors
Chronic pain conditions
Pain is one of the most common causes of insomnia. Up to 2/3 of patients with chronic pain conditions also experience sleep disorders (7)
Thyroid dysfunction
People with lower thyroid hormone levels (hypothyroid) generally have longer sleep latency, shorter sleep duration and lower satisfaction with the sleep quality (8)
GERD (Reflux)
Nocturia (peeing at night)
Leg cramps
Restless Leg Syndrome
Hot flashes & night sweats
The single biggest trigger of sleep problems in perimenopause and menopause
68% of hot flashes trigger awakening/lighter sleep within 4 minutes
Women experience many more hot flashes than they consciously register
Arousal response: physiological changes during hot flashes include increased heart rate and sweating
Creates vicious cycles of disruption and fragmentation
Melatonin & Cortisol Dysregulation
Age-related melatonin decrease disrupts circadian rhythms
Every cortisol elevation delays sleep onset and reduces overall sleep efficiency
Early morning cortisol rise triggers premature waking
The 3am Perfect Storm
The Cortisol Connection
Elevated baseline cortisol & CAR in perimenopause
Hot flashes are more common in the later part of the night
Hot flashes trigger additional cortisol release
Lifestyle & Environmental Influences
Caffeine
High intake and timing will Impact neurotransmitters even earlier in the day
Can increase sleep latency by 20-30 minutes
Alcohol
Shortens sleep latency but disrupts REM and deep sleep
Initial sedation followed by fragmented sleep and increase awakenings in second half of the night. Affects 70% of drinkers
Exacerbates anxiety and hot flashes
Increase in early morning awakenings
Suppresses melatonin production and will increase core body temperature
Even small amounts in evening can impair sleep quality
Evening Blue Light
Suppresses melatonin by up to 50%
Received from electronics (phones/TV’s etc) and LED lights
Social Jet Lag
Staying up past your normal bedtime for fun-time will disrupt your circadian rhythm
Swing or Night Shift
It is very hard for night shift workers to get enough sleep during the day. They get a daily average of two to four hours less sleep than normal.
Shift Work Disorder is a circadian rhythm sleep disorder characterized by sleep problems that stem from working long or irregular hours
The Biology of Sleep
To better understand what to do, know more about the biology of sleep. Only after I quit working as a staff nurse and started giving workshops on sleep did I really start connecting the dots between what happens to our bodies during burnout, the biology of our sleep and how those weave together resulting in bad (non-restorative) sleep.
Before you develop your sleep tool kit (The Wind Down Sleep Tool Kit included further down) so you can unwind from what is keeping you awake and align with your natural sleep rhythms, it’s important to better understand how your body should be functioning. It’s not about “forcing” sleep. It’s about reconnecting with your body’s innate wisdom--and creating the conditions for deep rest to return.
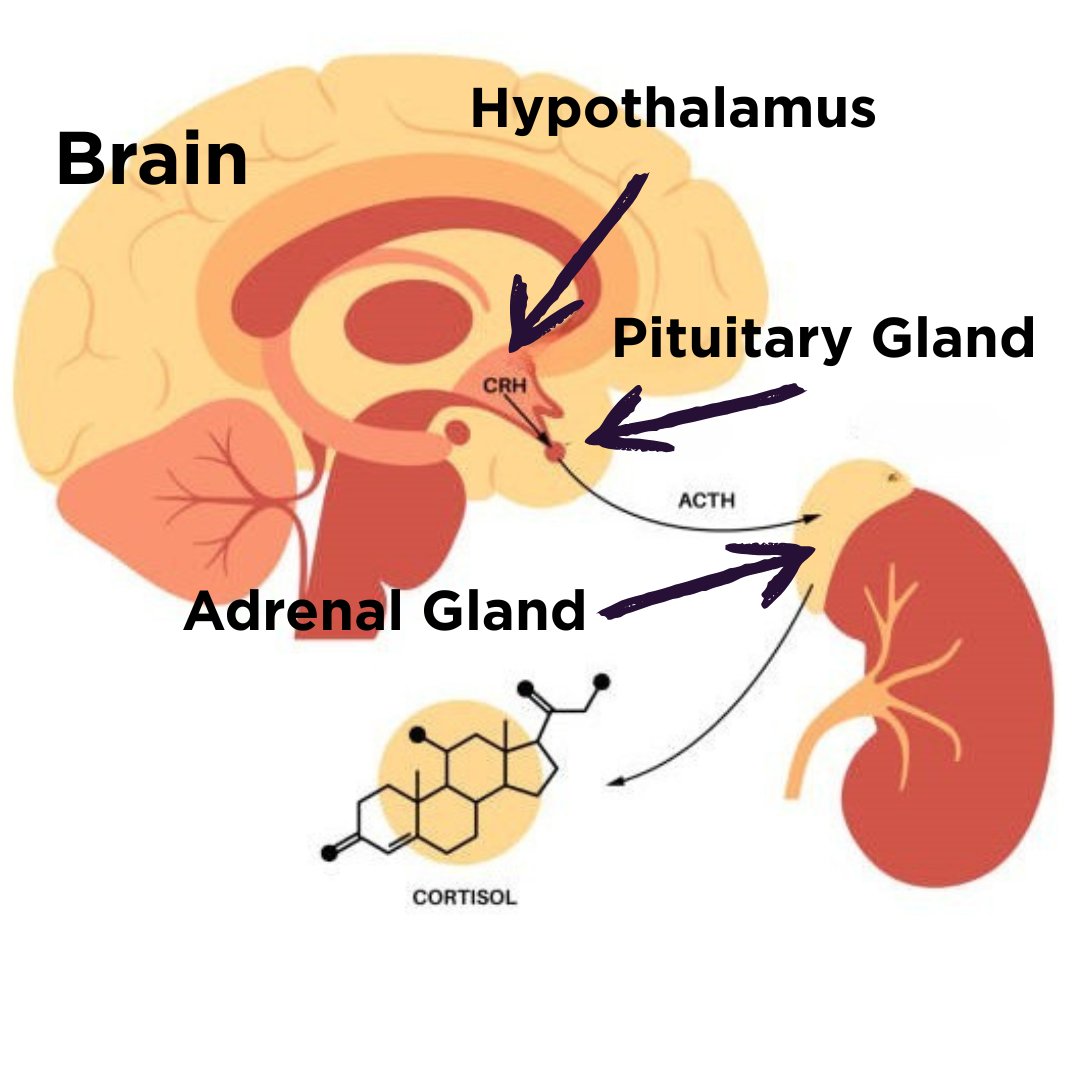
HPA Axis & Sleep
HYPOTHALAMIC-PITUITARY-ADRENAL AXIS
Diagram of the HPA Axis
What is it and why it’s important
It’s a cascade of endocrine (hormone) pathways that responds to specific feedback loops involving the hypothalamus (located in your brain), anterior pituitary gland (also in your brain) and adrenal glands (on top of your kidneys). Also known as a neuroendocrine communication system between these three organs that consists that release hormones into your blood in response to your nervous system (stress).
Regulates STRESS & SLEEP.
This hormonal feedback loop responds from increased stress (elevated cortisol levels) with decreased sleep quality and quantity, which can lead to increased stress and decreasing sleep even more.
Hypothalamus-keeps your body in a balanced state (homeostasis) for body temperature, hunger, mood, blood pressure, sex drive and sleep. It directly influences your autonomic nervous system and manages hormones. Releases corticotropin-releasing hormone (CRH) stimulating the anterior pituitary gland.
Pituitary gland-specifically the anterior pituitary gland is the conductor of your hormonal orchestra, directing other glands and tissues to make sure your hormones are working in harmony. Produces and releases ACTH which stimulates your adrenal glands to produce cortisol (stress hormone).
Adrenal glands-produces cortisol which controls blood sugar levels, supports metabolism, regulates blood pressure, suppresses inflammation, regulates your sleep-wake cycle and raises glucose levels under stress.
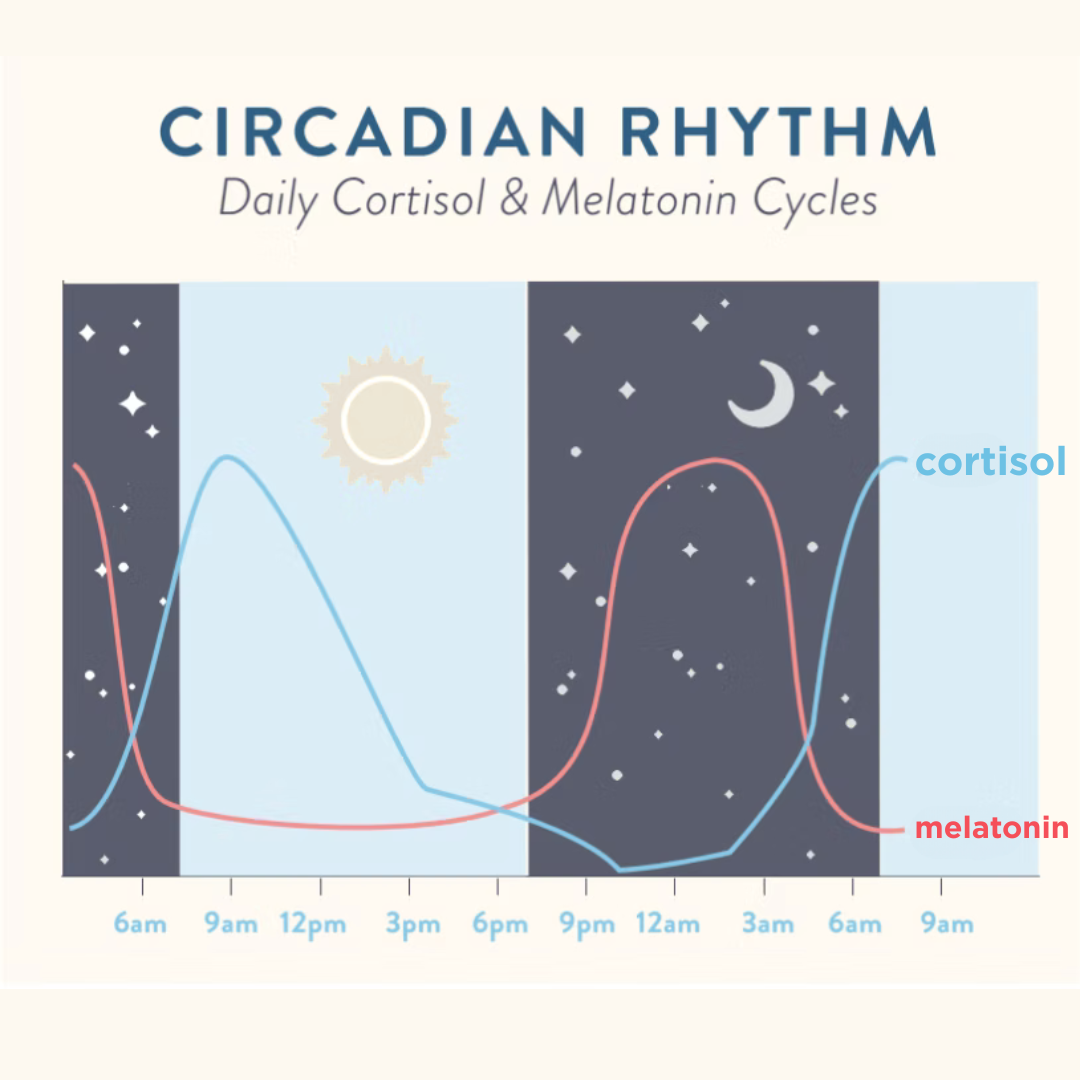
Circadian Rhythm
Circadian rhythms are 24-hour cycles that help govern essential bodily functions—especially the sleep-wake cycle—by syncing internal processes with the day–night cycle.
Cortisol & Melatonin Cycles
The Cortisol Awakening Response (CAR) is the predictable rise in cortisol within the first hour of awakening. There are two events that contribute to this dynamic rise in morning cortisol.
The first is in response to adrenocorticotropic hormone output from the pituitary as a part of the normal circadian activities of the hypothalamic–pituitary–adrenal (HPA) axis with involvement from the sympathetic nervous system.
The second occurs in response to exposure to daylight with the activation of the suprachiasmatic nucleus in the hypothalamus, which happens within 30-45 minutes after awakening and can increase cortisol by 50-60% from the waking value. These events take place in a timed and metered fashion, allowing for a rise and fall of cortisol over a one-hour period.
The purpose of the CAR is to mobilize glucose for energy needs, augment cardiovascular function, engage the motor system, and initiate and enhance cognitive processes that allow us to restore consciousness and engage in activity that requires us to be alert and ready for action (9).
Circadian Rhythm Cycles Flow Chart
Melatonin is a hormone produced by your pineal gland (located in the middle of your brain). As natural light dims in the evening, the signal to suppress melatonin decreases allowing melatonin levels to rise. This tells your body it’s time to relax and get ready to rest. The hormone secretion increases soon after the onset of darkness, peaks in the middle of the night, between 2 and 4 a.m., and gradually falls during the second half of the night.
Circadian Rhythm Bio-Clock
Case story
Client Jill S. (name has been changed to protect the innocent & exhausted) is a 39-year old nurse who’s been in the field for 11 years. She started working as a CNA and then got her nursing license and continued working on a cardiac step-down unit. Worked a 12-hour night shift for 8 years and struggled with chronic insomnia exacerbated by an autoimmune disease and medications.
Always felt tired and would sleep the whole next day-and-a-half after her last shift, could never get her sleep cycle regulated on her days off. Increasingly never had enough energy to see family and friends or do activities that she once enjoyed. Started having a lot of unmanaged anxiety the day before her first shift in her stretch about the patients she would have the next day, being able to get her work done and her manager had started micro-managing clock-ins and outs for any OT.
Three years ago she was able to switch to day shift with the hope that this change would improve her sleep. She did feel her sleep quality improved at first but she continues to wake up exhausted and struggles to make it through her 12-hour shift most days for the last 6 months. Every day at 3-4p, she feels her energy dip and concentration wane, wishing she was able to go home and go to bed. Instead, she is drinking a latte and eating a bag of chips to make it through the shift.
She came to me for help with chronic exhaustion, feeling too tired for her family and friends and always stressed about work.
Upon discussion, she decided her main priority was figuring out her sleep. We worked together to document her sleep pattern during working days and days off for two weeks. With this information we determined what specifically was preventing her from getting 8-10 hours of quality sleep. Her treatment plan:
Limit screen time (social media and bingeing Dexter) after work to minimize blue light exposure and doom scrolling for hours d/t being over-tired
Prioritizing winding down after her shift that emphasizes regulating her nervous system and feels supportive but easy
Easy nourishing meal that’s not fast food
Staying hydrated
Drinking Calm magnesium in 8 oz fluids when gets home to increase the depth of sleep
Using aromatherapy in car on way home and while at home
Started journaling 1-2 nights per week
By 9pm she will be off all screens and getting ready for bed whether she feels tired now or not but is maximizing the normal melatonin response around this time to re-train her body to become sleepy. She will use this time to journal, do deep breathing or listen to a sleep meditation.
By the end of three weeks after being mostly consistent with her routine, she started to notice a difference in the quality of sleep, she was not as tired upon waking and had stopped drinking caffeine in the afternoon (switched to herbal tea).
The Wind Down
Build Your Sleep Tool Kit.
Welcome to The Wind Down. Your sleep tool kit & guide to unwinding yourself and aligning with your natural sleep rhythms. It’s not about “forcing” sleep. It’s about reconnecting with your body’s innate wisdom--and creating the conditions for deep rest to return.
I want you to know:
You are not broken
You are not alone
Many parts of your life impact your sleep. Not everything you have control over so focus on what you CAN CONTROL and work from there. Your hormones will always be changing but you CAN influence them to bring them back to their natural flow & homeostasis. Sleep and stress are very intertwined in this aspect.
Now that I am several years past my own burnout and recovery, most mornings I wake up alert & rested. No longer is waking up tired, groggy and sluggish my normal like it was for the last 15 years. I usually know what happened for me to be waking up feeling sluggish whether it was a late night with friends, a series of days with eating convenience foods or staying up too late on my phone. The more mornings you have waking up rested, the more you want to prioritize making them happen more. This is here to help you.
Routines & Sleep Environment
Before bed routines and what you do upon waking up are very important. Our minds and nervous system thrive in consistency. No matter which shift you work, do very consistent things to tell your brain and body that you are slowing down and getting ready for bed —> sleep.
Before bed routine
Turn off or limit Blue light emitting devices
Do this after sundown or more realistically, within 1-2 hours before you are going to bed as blue light stimulates your brain
Use lamps that have soft warm light bulbs instead of LED
There is evidence that using red lights in the evening can help stimulate melatonin release (10)
Limit screen time
Social media increases anxiety and depression
No screens at least 1 hour before bedtime (including your reading tablet)
Prioritize regulating your nervous system and de-stressing
Calm your mind & unwind from your day
Practice Radical Rituals of Relaxation (see below)
Start your routine 1-2 hours before wanting to fall asleep
Keep it consistent but ok with flexibility
Get in bed 30 minutes before wanting to fall asleep
Journal your thoughts
Read a relaxing book (old school style, with actual pages)
Doodle
Coloring book
Calculate how much sleep you need/want
Plan your sleep routine accordingly (calculate backwards from the time you need to get up in the morning for 8-10 hours of sleep)
Consistency is key
Go to sleep around the same time each day
Build a consistent routine even if your shifts rotate or on swing or night shift. You are telling your nervous system and emotions—we do these actions and then go to sleep
Cozy bedroom with sleepy tea
Sleeping Environment
Where you sleep matters
Cool Temperature
The ideal temperature is 65-68F (15.6-20C)
Room is Dark
Black out curtains if necessary
Think of any light coming in through windows or from within the room
No electronics or phones
Avoid potential beeping, vibrations or alerts (unless you are on-call)
Don’t make it easy to grab your phone if you wake up in the middle of the night
Cozy bedroom with a wall of lights
Noise
White noise can be your friend if you are sleeping with the windows open (fans are great for this)
If you are super sensitive, consider noise cancelling headphones for sleep
Feels cozy to you
Your bedroom is your inner sanctuary, make it be yours
Love walking into your bedroom, be excited to lay in bed
Decrease or eliminate clutter
Clutter increases anxiety
Wake Up Routine
Young woman waking up in bed rejuvenated
What sound wakes you up?
This is how you start your day
Think of alternatives to the traditional alarm clock sound. My alarm clock sound is ocean waves, a gentle way to begin my day that my brain is alert to hearing and my nervous system benefits from not being jolted awake
There are light alarm clocks that progressively get brighter, mimicking the sun to wake you up
Natural light into your eyeballs before a screen
This helps regulate your circadian rhythm, influencing your hormones and your sleep pattern
Even if it’s dark, be looking at natural light before your screen
Wake up around the same time each day
How you start your day
Do you rush around in the morning?
If mornings are stressful, brain storm how it can be done differently so you are starting your day not from a place of chaos but creating space and time for your nervous system and you to be emotionally ready for the day ahead
Exercise
Move Your Body—Daily
Two women walking and laughing outside
Doesn't have to be strenuous. Or even breaking a sweat. Just move and stretch
Yoga
Tai Chi
Walking
Qi Gong
Ideally in AM or not too late in evening
Getting out in Nature is associated with increases in happiness, subjective well-being, positive affect, positive social interactions and a sense of meaning and purpose in life, as well as decreases in mental distress. And it’s just outside your front door
Stress Management
Nervous System Regulation
Stress increases your cortisol (the stress hormone) which disrupts your circadian rhythm. Regulating your nervous system is an important part of stress management and reducing your cortisol levels.
Hyper aroused state
Excessive activation in the form of fight/flight responses
Hypo aroused state
Freeze response, emotionally flat, lack of energy and response (functional freeze)
Goal —> Window of Tolerance
Optimal zone where you can deal with stress from every day life
Image from mindmypeelings.com
For more in-depth information, read this Connecting the Dots Series on Burnout, the Nervous System & You which goes in to detail about the different states, what they mean and how to regulate differently.
Learned Coping Skills
The tools you use to manage stress, even when you don’t consciously realize it. Many of these tools may mirror what your caregivers or parents did when you were a child. Even when you consciously choose differently, these are very familiar to your nervous system and emotionally, so it can be hard to change these habits. Be gracious with yourself but persistent.
Coping written out in wooden blocks on a clipboard
Adaptive (healthy coping mechanisms)
Behavior works to resolve problems using methods that reduce stress & harm
Enables people to adapt to stressors and challenges effectively. Promotes problem solving skills, emotional regulation and resilience
Maladaptive (unhealthy coping mechanisms)
Behaviors that do not always seek to resolve the problem but are usually attempts to reduce symptoms in the short term (not wanting to feel your feelings)
These can end up causing harm and increase stress in the long term
More in-depth information can be found in my Getting Beyond Burnout Workshop. Find the next available workshop HERE.
Radical Rituals of Relaxation
Create rituals out of every day actions that you do. Be intentional with this. Be mindful (simply aware and conscious) of what you’re doing and how you can make it NOT just something that you do every day but make it an experience.
Our bodies remember the trauma we experience, even when our minds do not
You CAN release this trauma—-the body keeps the score and the body can change the score
Water
Intentional baths-light candles, play soft music, add oil and essential oils to the bath
Showers-imagine the water washing away the stress
Being in, on or near bodies of water
Massages
If your insurance covers massage, why aren’t you doing them?
Deep breathing
Practice in times when you’re not feeling stressed
Slow deep breathing can activate the parasympathetic nervous system, bringing a feeling of relaxation and calmness
Acupuncture
It’s like a massage without the massage, deeply relaxing
Body oiling
This is not the same as using lotion on your skin
Use organic olive oil (see picture) and rub into your skin daily to nourish your skin and relax your muscles & nerves (even better if it’s infused with beneficial herbs)
Cold water immersion
Has been shown to have many health benefits, article for more in-depth information
If your dominate nervous system state is hypo aroused, not a good idea but if your normally in a hyper aroused state, can cool feeling so activated (immersing your hands in cold water if you are very activated or feeling chaotic or disconnected from yourself is a great way to bring yourself back into your body)
Journaling
Writing has the power to heal, offering a safe space to process emotions, reframe experiences, and gain deeper self-awareness
Get a super cute journal and fun colored pens
Time & Space to do NOTHING
Intentionally rest
Multi-tasking is a great way to get nothing done
Aromatherapy
Essential oils
Candles
Incense
Yoga Nidra
A sleep based meditation technique that allows effortless disengagement from the thinking mind by entering space between waking and sleeping
A practice that's especially effective at reducing stress and anxiety and can even help with insomnia
Guided meditations
A simple, fast way to reduce stress without getting so lost in your squirrel-mind while trying to do silent meditation
Insight timer app is a good one that is free
Somatic yoga
A practice that combines yoga with somatics—a type of movement therapy that retrains your brain and body to move and sense muscles. Although there is limited research on the benefits of somatic yoga, initial evidence suggests that it can help improve stress, reduce pain, and relieve trauma
Drinking herbal tea or black tea or even coffee
Make it a ritual
Engage the senses
Emotional Freedom Technique (EFT)/tapping
EFT is an alternative treatment for physical pain and emotional distress. It’s also referred to as tapping or psychological acupressure
Nourish Yourself
Sugar & Caffeine Cycles
Poor sleep can result in increased caffeine intake to stay away plus craving for simple carbs to fuel yourself
This is the 3pm afternoon crash
Even if you think caffeine doesn’t effect your sleep, it does
Eat to Nourish Yourself
When I was a traveler in my 20’s, I never brought food to work and would eat the meals not delivered left over from dayshift (sometimes ok but Kaiser SF had processed microwave meals for patients but I still ate it. Would not recommend.
Drinking Enough Water During The Day
Secondary benefit is you have to pee therefore making you take a break
Autumn outdoor table setting with fruit, cheese & wine
Alcohol Consumption (10)
Shortens sleep latency but disrupts REM & deep sleep
Initial sedation followed by fragmented sleep and increased awakenings in second half of night
Affects 70% of drinkers
Exacerbates anxiety & hot flashes
Increase early morning waking
Suppresses melatonin production and increase core body temperature
Even small amounts in evening can impair sleep quality
Processed Foods
The Wind Down: Your Sleep Tool Kit download
Click the unicorn to download your free 6-week guide to unwinding yourself and getting better sleep.
This 6-week guide is based on Cognitive Behavioral Therapy for Insomnia (CBT-I) and includes an assessment for insomnia and for burnout to give you information so you can use the best tools to get better sleep.
Botanicals & Supplements
Adaptogens & Nervines
No matter how busy life gets, it's essential to make time for yourself. Supporting our nervous systems is particularly important. Herbal nervines and adaptogens are invaluable allies for coping with the normal day-to-day aggravations of life: work pressures, family responsibilities, financial worries, seasonal mood slumps, over-reliance on caffeine, and so on. Whether your nervous tension results in intermittent minor aches, occasional functional freeze, or sleepless nights, herbs can help us find relaxation and calm to enjoy normal and healthful cycles of activity and rest.
Adaptogens
Adaptogens can non-specifically enhance the resistance of human body under a wide range of external stress conditions with a multi-targeted and multi-channel network-like manner, especially by affect the immune-neuro-endocrine system and the hypothalamic–pituitary–adrenal axis (12).
Herbs and supplements do have side effects and don’t work like pharmaceuticals. Do your research and take under the guidance of a qualified clinical herbalist or naturapathic doctor (ND). Your MD, ARNP or PA is not likely to have the herbal training and understanding.
Nervines
Nervines are herbs that specifically help support the nervous system. They are used to help relieve normal muscle tension, circular thoughts, wakeful nights, and the occasional worry we all experience from time to time. Some of these herbs provide multiple nervine actions. Skullcap is one such herb: it helps reduce muscle tension, calm worried thoughts, and also nourishes the nervous system. Others, such as oat tops, are not necessarily noticeably relaxing to the physical body, but help support healthy nerve function with regular use.
Ashwagandha
Maca
Eleuthero (Siberian Ginseng)
Tulsi (Holy Basil)
Schisandra
Reishi & Lion's Mane Mushrooms
Rhodiola (Golden/Arctic Root)
Dong Quai (Angelicae Sinensis)
St John's Wort
Lemon Balm
Rose
Lavender
Nutmeg
Chamomile
Elderflower
Milky Oats
Skull cap
Catnip
Valerian root
Hops
Sleep Specific Botanicals
Valerian Root
Chamomile
Peppermint
Lemon Balm
Lavender
Nutmeg
Passionflower
Hops
CBD
California Poppy
Catnip
Skullcap
Most of these herbs can be taken as teas, tinctures, capsule form, herbal body oils, and herbal vinegars. For more in-depth information, attend the next Herbal Medicine: Botanical Support for Stress & Overwhelm. This quarterly webinar will discuss how to access and use these herbs beyond dried, ground and in a capsule to swallow.
Supplements
Magnesium
Melatonin
B Vitamins (esp B6 and B12)
GABA (Gamma-Aminobutyric Acid)
5-HTP (5-Hydroxytryptophan)
L-theanine
Glycine (2-Aminoacetic Acid)
Calcium
Zinc
Sleep Disorders
Medical Diagnosis
Insomnia
Obstructive Sleep Apnea
Jet Lag Disorder
Restless Leg Syndrome
Shift Work Disorder
Advanced Sleep Phase Disorder
Delayed Sleep Phase Disorder
Non 24 hour Sleep Wake Disorder
Irregular Sleep-Wake Rhythm Disorder
Narcolepsy
Snoring
There is hope.
As you see, there is a lot that goes into your sleep. Whether you’re sleeping well or not. There’s also a lot you do have control over and can influence though it may seem like you don’t. It is very overwhelming and can seem hopeless but I want to give you hope that even small changes will have a ripple effect for positive change. Many people struggle with sleep even intermittently. And then there’s no understanding of why some sleep is good and others is not. My hope is that this really long intense article connects those dots so you can sleep better on most nights, if not every night. Here’s to you having the best sleep every night that you can.
Personal sleep coaching
If you continue to struggle with sleeping and would like some additional help and guidance, I offer sleep coaching.
Schedule your free consult today for better sleep tomorrow
Change your sleep, one day at a time over water ripple
Tool Integration Sessions
There’s a gap between knowing the tools to regulate your nervous system & cope with stress to implementing them. This session is designed to close that gap.
Offered twice monthly, virtually and locally with-in the Pacific Northwest in-person (great for friend groups, your department or floor-email me hello@moonshinewellnesspnw.com).
Virtually every 2nd & 4th Thursday evening of the month at 7pm (Pacific).
References
Prevalence and associated factors of insomnia symptoms among doctors and nurses under the context of high prevalence of multiple infectious diseases: a cross-sectional study; Front Public Health. 2024 Aug 29;12:1423216. doi:10.3389/fpubh.2024.1423216
Relation between Burnout and Sleep Problems in Nurses: A Systematic Review with Meta-Analysis; Healthcare (Basel). 2022 May 21;10(5):954. doi:10.3390/healthcare10050954
Nursing 2025: No Relief as Burnout, Stress and Staffing Woes Persist; Cross Country Healthcare and Florida Atlantic University’s Christine E. Lynn College of Nursing
Primary Insomnia: A Lifelong Problem; Heidi Moawad, MD; September 11, 2020
Secondary insomnia: diagnostic challenges and intervention opportunities; Christina S. McCrae and Kenneth L. Lichstein; Sleep Medicine Reviews, Vol. 5, No. 1, pp 47–61, 2001 doi:10.1053/smrv.2000.0146, available online at http://www.idealibrary.com
What doctors wish patients knew about insomnia; By Sara Berg, MS; Apr 25, 2025
How to Beat Insomnia When You Have Chronic Pain; The Cleveland Clinic; August 10, 2020
Thyroid Dysfunction and Sleep Disorders; Max E Green, Victory Bernet and Joseph Cheung; Front Endocrinol (Lausanne). 2021 Aug 24;12:725829. doi:10.3389/fendo.2021.725829
Anxiety, Depression, and the Cortisol Awakening Response; Tracy Tranchitella, ND; July 23, 2021
Helping Women Sleep Well in Perimenopause & Menopause webinar; Dr Aviva Romm; May 5th, 2025
What Color Light Helps You Sleep?; Written by Jay Vera Summer | Medically Reviewed by Pranshu Adavadkar, MD; July 2025
A preliminary review of studies on adaptogens: comparison of their bioactivity in TCM with that of ginseng-like herbs used worldwide; Lian-ying Liao , Yi-fan He, Li Li , Hong Meng, Yin-mao Dong, Fan Yi, Pei-gen Xiao; Chin Med, 2018 Nov 16;13:57. doi:10.1186/s13020-018-0214-9